We search every gene in the genome to program immune cells and overcome the limitations of current therapies.
For scalable cell therapies that may cure cancer, we combine safe targets, next-generation cell programming, and off-the-shelf (allogeneic) T cells.
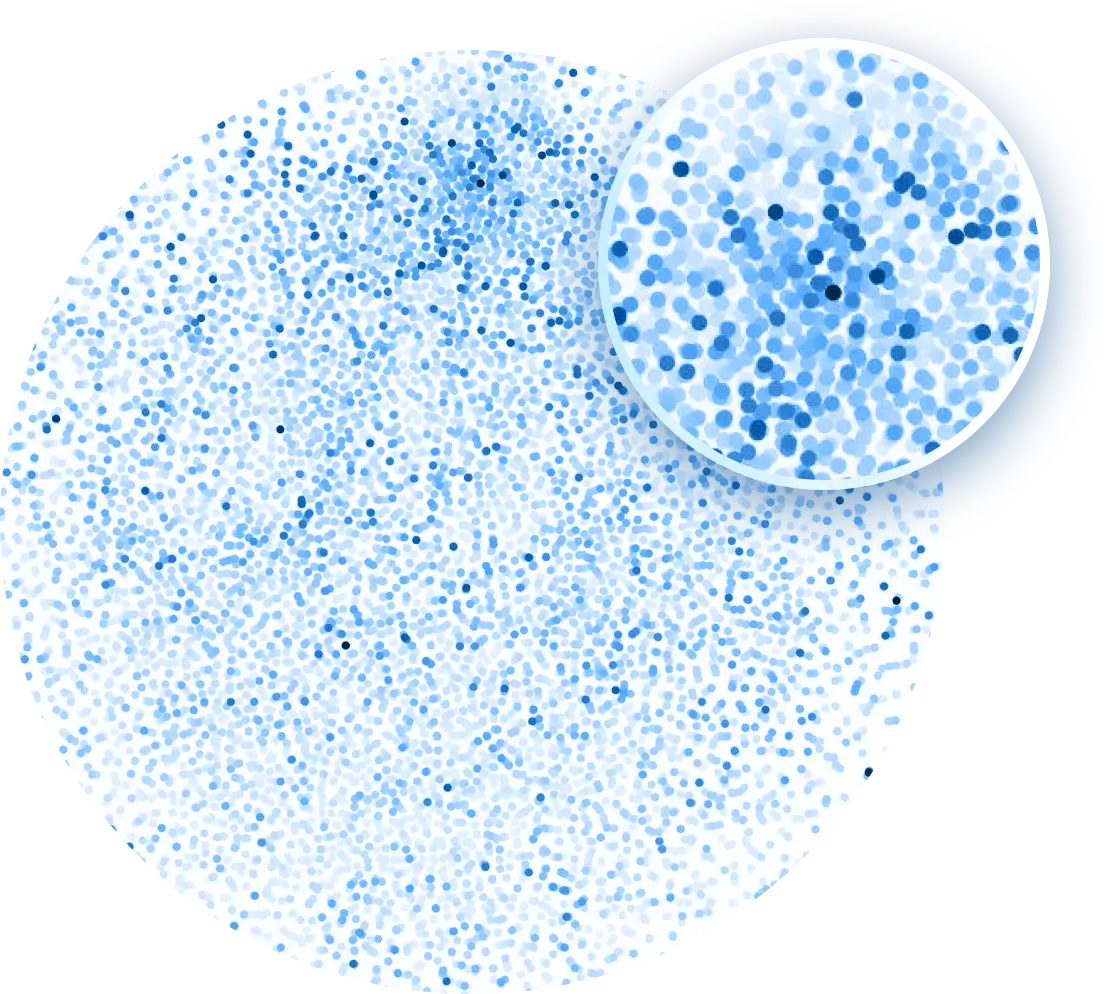
Traditional approaches to armoring cell therapies just look under the lamppost — at what’s already known. With our DNA-barcoded, massively-parallel overexpression platform, we test thousands of genetic payloads in T cells.
Which genes make T cells more persistent? Resistant to immunosuppressive factors in the tumor microenvironment? Evade immunosuppressive regulatory T cells or macrophages? Eliminate tumors?
Our unique datasets connect thousands of genes to key immune phenotypes, encompassing millions of genotype-phenotype pairs. This expanded universe leads to new discoveries and better T cell programming to achieve deep and durable activity against cancer.

Current AI protein design methods are limited by training data, which is mostly focused on protein structure. Superior data makes for surprising discoveries and superior therapies: OverT uses AI and ML approaches trained on disease-relevant phenotypes generated using our unique platform to find optimal T cell programs.
This includes combinations of gene programs that work synergistically and synthetic proteins that outperform natural versions.
Using patient samples and data, we identify superior receptors for cell therapy. OverT’s chimeric antigen receptors (CARs) outperform the drugs tested in the clinic with better on-target activity and higher specificity.
We are also identifying new, safe T cell receptors (TCRs) via single-cell screening of thousands of T cells from cancer patients. These TCRs can be used in any patient as they are not restricted by the genetically diverse MHC molecules.
In each single-cell experiment, we not only identify these receptors but quantitatively assess their ability to eradicate many different tumors.

Today’s cell therapies are expensive and labor-intensive. They require shipping patient cells to the lab for genetic modification, extensive safety testing, and then shipping them back to the patients.
What if cell therapy had the scalability of more conventional drugs like antibody-based therapies? We reduce the time to treatment with a naturally allogeneic, off-the-shelf therapy.
We pair the advantages of cell therapy (one time treatment with a curative potential) with the scale of biologics, shortening patient waiting time, expanding access, and making the therapy more affordable.
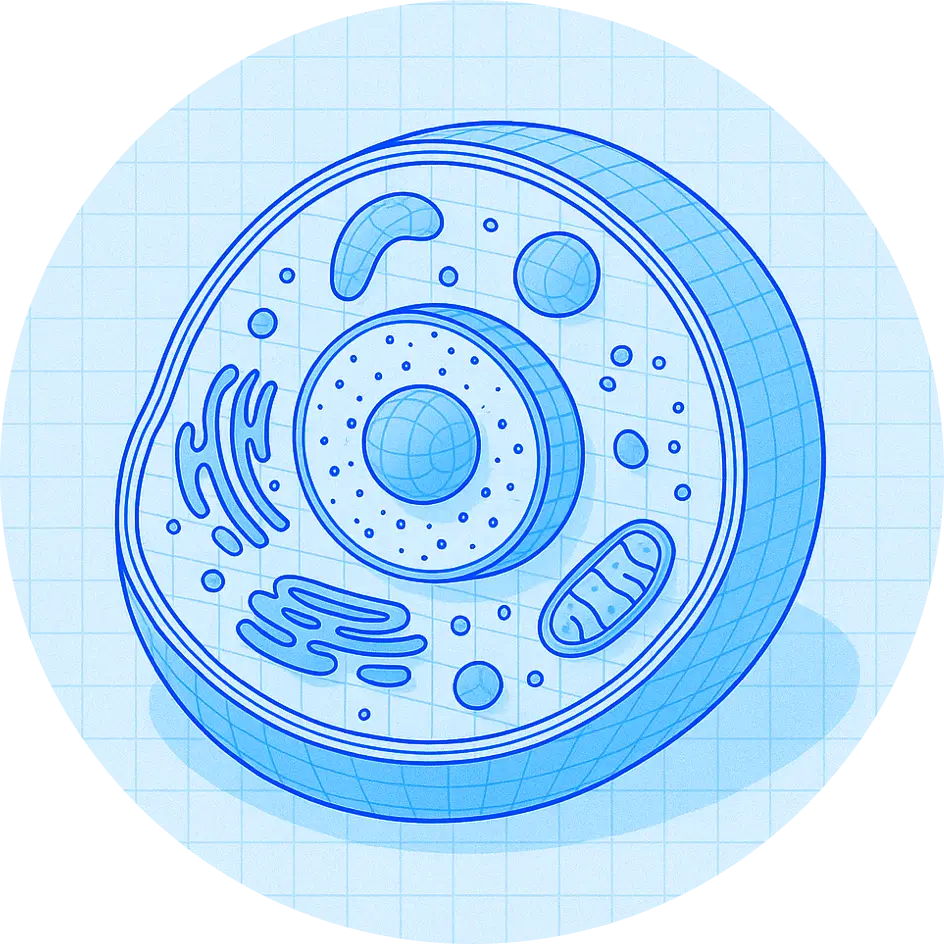
γδ (gamma delta) T cells are a unique and powerful subset of T cells. They provide the chassis to carry OverT’s receptors and programming. They are safer because they are naturally allogeneic — no gene editing required.
With γδ T cells, there is no graft-versus-host disease and they have less toxicity than autologous CAR T. They hone-in on tumors due to their innate affinity for tissues, making them an ideal immunotherapy for solid tumors.
Several studies have found an association between γδ T cells and better long-term survival of cancer patients. They are as scalable as a biologic: OverT’s team has developed new processes to manufacture γδ T cell-based therapies at scale.
Historically, γδ T cells have not been widely used for cell therapy because they don’t survive in vivo for extended periods. However, with OverT’s programming, γδ T cells become just as persistent and powerful as conventional T cells, paving the way for new opportunities in cell therapy.
Chowdhury, S., Kennedy, J. J., Ivey, R. G., Murillo, O., Hosseini, N., Song, X., Petralia, F., Calinawan, A., Voytovich, U. J., Savage, S. R., Berry, A., Reva, B., Ozbek, U., Krek, A., Ma, W., da Veiga Leprevost, F., Ji, J., Yoo, S., Lin, C., … Paulovich, A. G. (2023). Proteogenomic analysis of chemo-refractory high grade serous ovarian cancer (PTRC-HGSOC) (Version 1) [dataset]. The Cancer Imaging Archive. https://doi.org/10.7937/6RDA-P940